Dispatch #1: What ails India's healthcare?
Part 1 of the series that looks into India's public health system
The COVID-19 pandemic has brought the conversations on India’s healthcare back to the mainstream. Earlier the discourse on public health in India was relegated to episodic outrage only when there were child deaths in a public health facility or when the poor have to carry the corpse of their loved ones because of the absence of an ambulance or a hearse van. But the pandemic has forced us to think about India’s health system and whether it can endure another onslaught of zoonotic disease.
The pandemic has exposed the weak capacity of India’s public health system. The result of the perennial neglect of the healthcare system is out there for us to see when the health facilities and the health workers are struggling to control the spread of the pandemics.
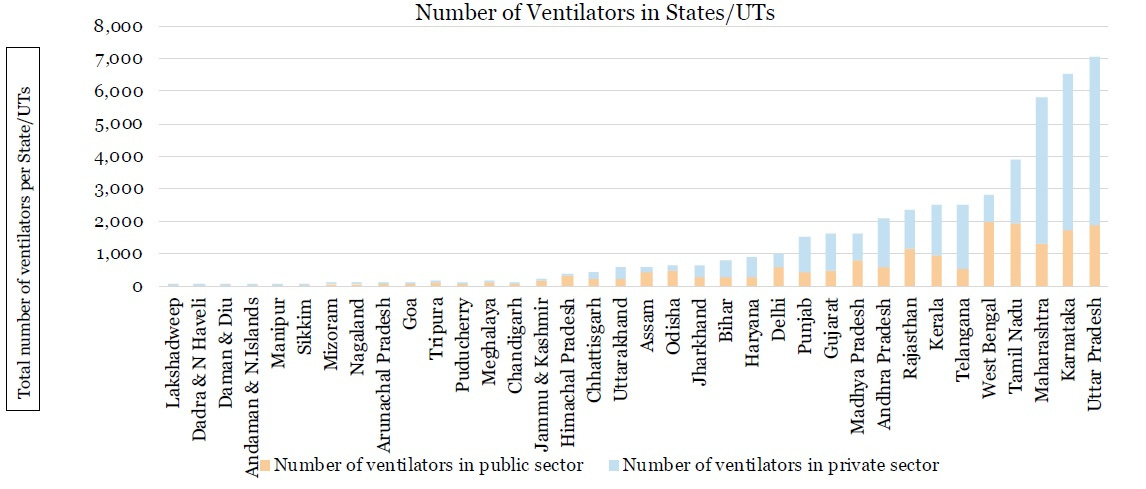
In an analysis, published in April, the Princeton University and the Centre for Disease Dynamics, Economics & Policy estimated that India has 19 lakh hospital beds, 95 thousand ICU beds and 48,000 ventilators. Most of this infrastructure is concentrated in the private sector.

Most of the hospital beds are concentrated in 5 states- Uttar Pradesh, Karnataka, Maharashtra, Tamil Nadu and West Bengal. The maximum number of hospital beds in these states are with the private sector.

A similar trend can be seen for the number of ICU beds and the ventilators.
Why don’t Indian voters penalise political parties for this neglect?
According to ADR’s ‘All India Survey on Governance Issues and Voting Behaviour 2018’ there is a huge gap between voters’ priorities on specific governance issues and the government’s performance on those issues.

Out of the top ten governance issues, better healthcare came second as voters’ priorities, after better employment opportunities. But the score given by the voters on the government’s performance on providing better healthcare was below average (2.35).
In 2004, two World Bank economists, Stuti Khemani and Philip Keefer tried to explain as to why do the poor in India get poor services and why don’t they penalise the political parties for not providing basic services like healthcare. They argued that broadly there are three reasons that explain inadequate and poor-quality public services in India- focus on narrowly targeted goods to interest groups (club goods), lack of credibility of political promises to provide public goods rather than the targeted transfer of goods and social fragmentation.
The poor state of India’s public health system
A Newsclick analysis of India’s public health system shows the glaring gaps in healthcare delivery. The article has used the National Health Profile 2019 and NSSo data for the analysis.
a) The infrastructure disparities are evident across regions and states. As per the WHO, the recommended doctor-population ratio is 1:1000 and one hospital bed should cater around 400 patients. While the Southern states have done relatively better than the rest of India in terms of doctor-population ratio, the population-government hospital bed ratio in all the states is not even remotely close to the recommended number.

b) Due to the poor quality of services, inadequate infrastructure and man-power, people opt for private hospitals which is costly and that increases the out-of-pocket expenditure. Across all the states, private care providers dominate the out-patient and in-patient care.


c) The per capita expenditure on healthcare by most of the states is lower than the national average of Rs 1,739. Since government spending is low, the out-of-pocket expenditure is high.

According to the calculations in this HT article, the child mortality rates are lower in states that have an adequate number of doctors.
States such as Madhya Pradesh and Bihar, which have a lower share of doctors, also have higher child mortality rates. In contrast, southern states such as Kerala and Tamil Nadu fare well on share of doctors and child mortality.
The Rural Health Statistics report by the Health Ministry has also pointed out the acute shortage of specialists in public health facilities in rural India. No points in guessing that the states that have the maximum number of specialists shortage are the same that have the maximum number of child mortality rates.

Using the NFHS-4 data, the article claims that the poor as per the wealth quintiles and the historically marginalised groups of SCs and STs bear a disproportionate burden of poor provision of health care services.
The burden of poor provision of social services such as health care has a skewed impact beyond class lines. Because the caste hierarchy in India is closely linked to economic backwardness, those at the bottom of the social ladder bear a disproportionate burden of poor provision of health care services. Child mortality is the highest among households not just in the lowest wealth quintile, but also Scheduled Castes and Scheduled Tribes, which are the most backward social groups. These indicators are the best among households belonging to upper castes and highest wealth quintiles.

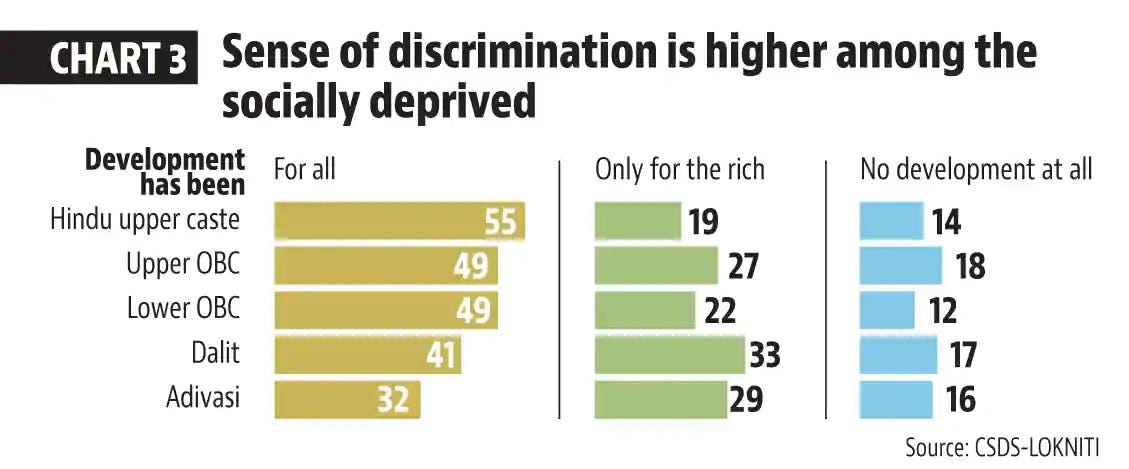
These trends are quite puzzling. While on one hand, it’s the socio-economically backward sections of the society that suffer a lot because of poor provisioning of basic services such as healthcare, on the other hand, the political actors are not punished for not being able to provide basic services such as health, education and sanitation.
What is more surprising is the fact that they know very well that the ‘vikas’ that was promised to them has not benefited them at all. According to a pre-poll survey from the National Election Study done by the CSDS, the feeling that the development is not inclusive is more within the socio-economically backward communities.
Oxford University scholar, Tanushree Goyal, in her paper titled ‘Do citizens enforce accountability for public goods provision? Evidence from India’s rural roads program’ writes that the Indian voters do not necessarily vote on development issues or public goods provisioning. Her study is around the flagship Pradhan Mantri Gram Sadak Yojana (PMGSY) that provides all-weather roads to the villages in India. Even though the rural roads have made access to the markets and basic services like schools and health centres easy, the voters do not reward the incumbent governments. Voters respond to the caste affiliations rather rewarding the political actors on the basis of public provisioning.
In a blog, Goyal wrote about the implications of her study for Indian democracy and politics of development, ‘The findings have important implications for democratic governance amongst, other debates. With the rise in infrastructure provision in many countries in Africa, these findings should worry scholars of democratic governance. Electoral incentives, generated through accountability mechanisms, are posited as a key means of improving service delivery in developing democracies. However, if voters remain unresponsive to policy provision, electoral incentives for public goods provision or improving service delivery, may diminish over time, leading to abandonment or poorer implementation of these crucial programmes.’
In a paper titled ‘Growing Cleavages in India? Evidence from the Changing Structure of Electorates, 1962-2014’, Abhijit Banerjee, Amory Gethin and Thomas Piketty have argued that the BJP came to power because of the support of its traditional vote bank comprising of Brahmins and other Forward Castes. Hence the main factors that determine voters’ preference for a political party in India are caste and religious identification.
In the next dispatch, we will discuss more on what ails India’s healthcare. We will also talk more about the politics of public provisioning in India.
Further readings:
1) Indians Tend Not To Vote For Development: Study
2) Indians vote on caste, religion because they lack information on MP, MLA performance: Study

