Dispatch #2: What ails India's healthcare?
Part 2 of the series that looks into India's public health system
There is a fundamental difference between ‘public health services’ and ‘medical services’.
‘Public health services reduce a population’s exposure to disease through such measures as sanitation, vector control, disease surveillance, food safety, waste disposal, monitoring water systems, health education to improve personal health behaviours and implementation of basic public health regulations’, explains demographer Monica Das Gupta of Maryland University.
These are different from the medical services that are individual focussed and consist of health facilities and care providers. According to Das Gupta, public health services consist of a whole range of services- improving slaughterhouse hygiene, monitoring water bodies and ensuring vector control, maintaining food safety standards, health promotion etc. These services have positive externalities and provide ‘public goods’.
These services are largely invisible to the public, the public only becomes aware of the need for them when a problem develops (when an outbreak happens). Yet unlike most medical services-which focuses on the needs of the individual patients- these services are of high priority for assuring good health for a population as a whole.
It has been long been accepted that the most effective approached to improving population health are those that prevent rather than treat disease. It is the norm for public health services to be publicly funded since the market has limited incentives to provide them.
- Monica Das Gupta
The West realised the importance of public health services after a series of big health shocks like the cholera epidemic in 19th-century London and the Spanish flu in the early decades of the 20th-century. The advent of germ theory and the pioneering work of John Snow, Robert Koch, Louis Pasteur, Leeuwenhoek among others made the societies and the governments realise the importance of investing in public health systems like sanitation and disease surveillance.

Nobel laureate Angus Deaton has written about the public health movement in Europe, in his book ‘The Great Escape: Health, wealth and the origins of inequality’.
The major credit for the decrease in child mortality and the resultant increase in life expectancy must go to teh control of disease through public health measures. At first, this took the form of improvements in sanitation and in water supplies. Eventually science caught up with practice and the germ theory of disease was understood and gradually implemented, through more focussed, scientifically based measures. These include routine vaccination against a range of diseases and the adoption of good practices of personal and public health based on the germ theory. The improvement of public health required action by public authorities, which required political agitation and consent and could not have been accomplished through the market alone.
The improvements in sanitation, followed by measures based on the germ theory of disease, were the major factors in improving life expectancy in northwestern Europe and in the British offshoot countries.
- Angus Deaton
It was not only the pandemics that forced the developed world to adopt public health services. There were two other major concerns- crowding of the cities because of the Industrial Revolution and the increase in the number of deaths in the armies because of the outbreaks. The pressure on the governments mounted because not only the rich but the poor also suffered. This was the time when antibiotics were not yet discovered. “The realisation that germs are responsible for communicable diseases gave an impetus to the ‘sanitary movement’ which sought to remove these sources of diseases”, adds Das Gupta in her paper.
The sanitary movement involved radical changes in citizen’s belief about disease causation and in their health behaviours. Several measures were taken like installing latrines in the homes, giving up keeping livestock in urban homes and slaughterhouse hygeine. These measures brought about rapid declines in mortality and morbidity. A large literature confirms that the development of these services was a critical part of the health transition in a large number of present day developed countries.
- Monica Das Gupta
Japan, who was aspiring to become a world power in the 20th-century, adopted most of these European public health measures in the colonies as well in Korea and Taiwan. As a result the health indicators of these countries, have always been better than South Asian countries.
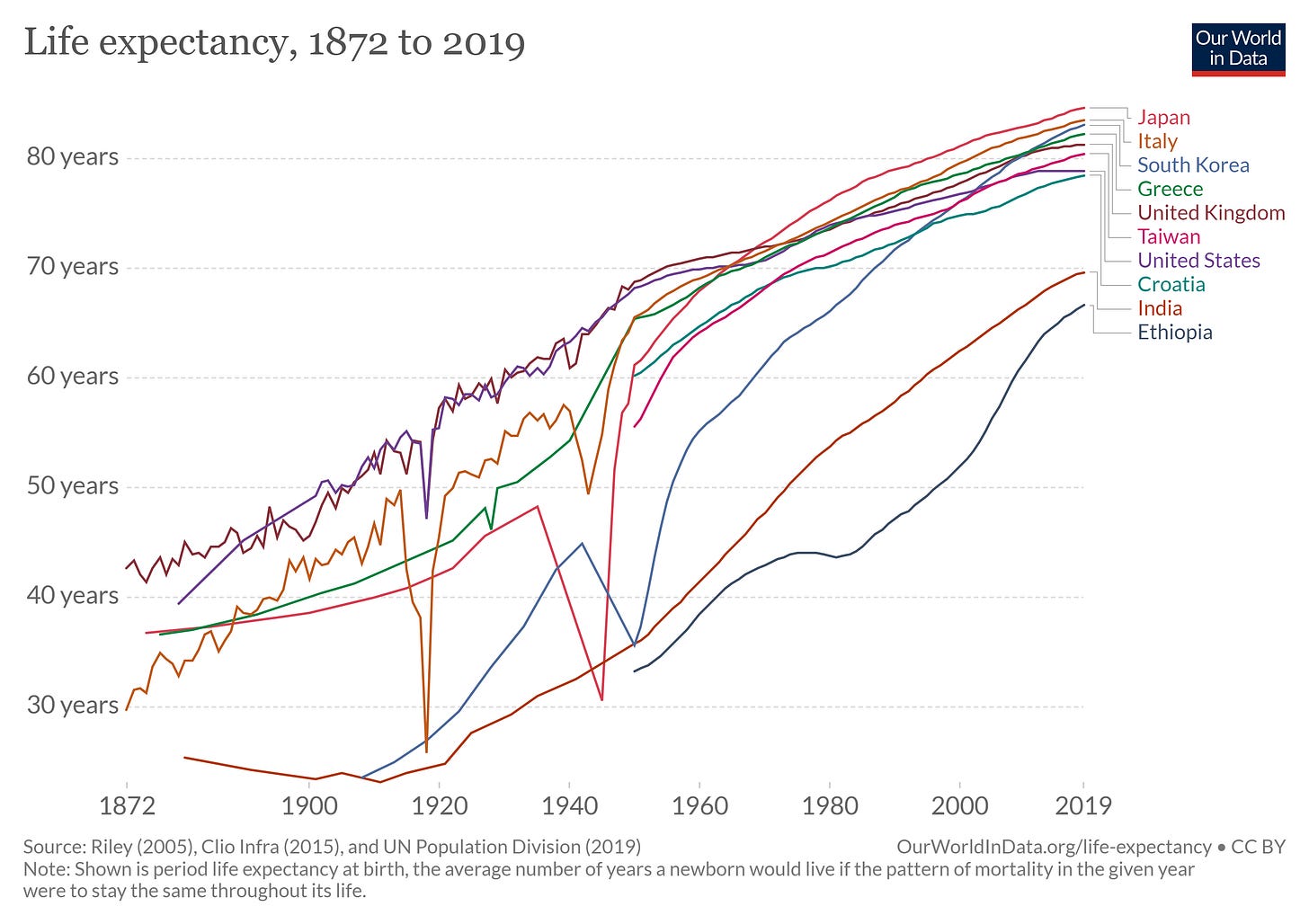
The life expectancy in European countries, Japan and its colonies started to improve from the 19th-century onwards and has always improved except the decline during the two World Wars. India started from a very low base and has not done much progress when compared with these countries. In 1940, the life expectancy of Japan, Korea and Taiwan was 50 years, while in India the life expectancy was 32 years.
In India, some of the public health measures were in place, but only in cantonment areas where the British soldiers were housed or in the British residential areas. The public health systems were only protecting the British at the cost of the natives. After independence, the public health systems in India were gradually dismantled and the medical services with a heavy focus on curative health started to dominate. Public health measures like sanitation, health surveillance, health promotion etc. never became priorities in our health policies.
A lot of this has to do with the nature of public health services. The success of public health services is negative in nature- an outbreak averted, a plague controlled etc.- that doesn’t make for good optics for politicians when compared with a more visible and tangible tertiary hospital or a dialysis centre. In a noisy democracy like India, behind the scenes and quite public health measures do not get traction from the political parties and hence do not make their way to the election manifestos when compared with the promises of opening an AIIMS or a medical college in a state. Similarly, toilet construction, a visible output, becomes central to the sanitation policy while ignoring sticky issues like usage of toilets, behavioural change, size of the pit, disposal of the waste and the plight of sanitation workers.
The costs of this neglect have been high. As the COVID-19 cases are rising with each minute, deaths due to communicable diseases in India have always been high. Respiratory diseases and pneumonia, symptoms common to COVID-19 cases have been the biggest killers in India. According to the National Health Profile-2019, in the year 2018, 50% of all the deaths were due to respiratory diseases and pneumonia.


In the data, given below, from the Global Burden of Disease study, two of the top-5 killers in India are communicable diseases.

The number of deaths per 100,000 in India due to communicable diseases like lower respiratory infection, diarrhoea and TB is higher than the other low and middle-income countries.
Why hasn’t there been a demand for robust public health systems in India? Why the democratic institutions in India have not been able to put pressure on the governments to deliver on public health? Why has a three decade long sustained economic growth not been translated to better public health provisioning?
Das Gupta cites two reasons for this:
1) Low demand for public health- As discussed above, public health measures lead to negative results like the decline in child deaths from water-borne diseases. Hence it does not become an attractive proposition for political actors to sell this ‘behind-the-scene’ non-glamorous activity to the voters since the outputs are not tangible.
Imagine a politician talking about how the disease surveillance system set-up by the government helped prevent a rodent based epidemic in the capital city. But when the same politician will talk about spending health budgets in setting up hospitals that provide tertiary care (private good) or setting up medical colleges where the middle-class can send its children to study medical education at subsidised rates, then that becomes a unique selling proposition which leads to more demand of such interventions at the cost of public health measures.
The electorates typically prefer public funds to be used to provide private goods (such as medical care), rather than public goods (such as sanitary measures to protect the health of population)
-Monica Das Gupta
2) Elite capture- In India, like in most of the developing countries, the elite have played a major role in setting up the mandate of public policies. The neglect of primary health and primary education in India, while funding tertiary care health facilities and institutions of higher education, is one such manifestation. Gramsci has called this the ‘passive revolution’ which essentially means social transformation championed by the elite of the society that serves the purpose of the same elite leading that change.
High economic growth in India did not lead to basic provisioning of services like health and education. In a 2002 paper titled ‘Growth Without Governance’, authors Daniel Kaufmann and Aart Kraay argue that in some context higher economic growth may actually lead to institutional degradation because of the ‘elite influence and state capture’.
One possible explanation for negative feedback from per capita incomes to governance is the phenomenon of state capture. If the fruits of income growth largely accrue to an elite which benefits from misgovernance, then the otherwise possible positive impact of income growth on governance could be offset by the effect of elite’s negative influence.
-Daniel Kaufmann and Aart Kraay
If neither the democratic institutions nor high economic growth translates to good governance and public service provisioning then what does?
Lant Pritchett has argued that for a strong state capacity to deliver healthcare and education, there should be ‘thin accountability’ and ‘thick accountability’. Thin accountability essentially encompasses real tangible and observable features like presence of healthcare staff, infrastructure, expenditure per student, class size, enrollment ratio etc. Thick accountability consists of monitoring non-tangible complex features such as quality of care, learning outcomes etc. Indian institutions, to a certain extent, have been able to enforce thin accountability but they have a very long way to go to enforce thick accountability.

